Home Healthcare
Visionwest Home Healthcare has had a challenging but successful year. Funder eligibility and assessment policy changes altered normal growth patterns and the sector still hasn’t achieved sustainable funding.
Alongside this, the completion of the successful Home Healthcare technology programme that commenced in 2023 has created a challenge in how to get the best benefit out of the new technology and the wealth of data which we now have. We have now made significant strides in embedding the use of this technology and information and are using it to help drive operational decision-making and the growth of Home Healthcare.
Alongside these challenges, there are some amazing encouragements to share.
The team at Visionwest Home Healthcare supports people through:
- Home and community support for older people, people with injuries, people with long term chronic health conditions and tangata.
- Individualised Funding Host services.
Number of people receiving in-home support

Clients receiving disability support

Accessing individualised funding through Visionwest
Clients seeking support for injury recovery
Events of Significance
A number of innovations and changes have been instrumental in enabling better efficiencies and effectiveness in our service delivery, especially around our technology offerings. Significant steps taken over the past 12 months include:
- Our successful tender for ACC Funded Maximise Independence Services is a hugely significant moment for Visionwest Home Healthcare. Up until gaining this contract, we could only provide care to ACC clients through a subcontract to another provider and therefore had no direct relationship with ACC. As a direct provider of Maximise Independence Services, ACC Case Managers can choose to refer clients directly to Visionwest Home Healthcare. Full details of the gaining of this Contract are included in the Milestones section of this Report.
- The development and implementation of a new suite of operational dashboards in GoldCare, our client relationship management system (CRM). These dashboards replace the use of a large number of spreadsheet-based reports reports which required analysis prior to any operational use and therefore were difficult to use. The new dashboards embedded in GoldCare enable easy access to live information on most of the aspects of the work we do in onboarding and assessing clients and providing support services to them. The dashboards are tailored for the different work that each type of employee does, for example coordinators can better track coordination tasks and the work of our support workers, Care Managers can track where clients are at in the onboarding or review processes and team leaders can better track resolution of complaints and events. We plan to keep on developing these new reporting options alongside improved trend reporting created by the Insights and Analytics team.
- Early in the year we achieved our goal of distributing phones to 100% of Support Workers. Last year, our Annual Report described the rollout of the MobilityPlus App – an online tool that enables efficient and effective live communication between Support Workers and their Coordination Team resulting in consistent and well organised service delivery. All our Support Workers have now been supplied with phones and have been trained in the system. We have had overwhelming feedback that support workers love the new devices and the MobilityPlus App as they have better access to the information they need.
- Lakes region have had a 30% increase in volumes during the last year (from 5000 hours per month to 6500 hours per month). This has been created through significant work from our team in providing a high-quality responsive service that people want and need.
- The completion of mapping of a large number of our SOPs (Standard Operating Procedures) which relate to our system use. This has resulted in an improvement to our training and the standardising of many practices and our data capture across all of our teams. This is very much a ‘business improvement win’ but it is significant step forward for our staff and our day-to-day running.
Support Worker Graduations
Representing Visionwest Home Healthcare at a Expo.
Support Worker Christmas Function, Auckland.
The programme focuses on providing new employees with a better way of commencing employment with Visionwest Home Healthcare, giving them the skills they will need to be a successful staff member. It uses a multitude of different ways of learning to best meet the learners’ needs – we are already looking forward to describing it more fully in next year’s Annual Report.
The cancellation of two pay equity claims (that affected Home Healthcare) without a clear way forward was disappointing. Over the past three years, Visionwest put significant resource into this claim with the hope that we would be funded to meet a potential pay equity settlement. We continue to advocate to government in this area with the hope that a claim can be fully assessed and a settlement reached.
Angela’s Story
Navigating disability support can be overwhelming. For Angela, Visionwest became more than a service provider – it became a place of understanding, strength, and guidance.
Customer Relationship Management (CRM)
As alluded to above, the use of the MobilityPlus app and mobile devices are now fully embedded in our daily practices and the work lives of our Support Workers and Coordinators. Our new and improved GoldCare system has streamlined our processes and, alongside mobility, offered support workers paperless support for scheduling and client referrals.
With the total adoption of GoldCare and MobilityPlus, we are now completely digital with our coordination of services and recording of workday aspects such as times spent with clients and travel times between clients. This has revolutionised the work of our coordination and payroll teams and we are busy planning steps of how we can utilise the technology to improve work efficiencies and support better outcomes for clients.
Over 1,300,000 hours of support
Once again, Visionwest has delivered over 1.3 million hours of in-home healthcare this past year. We started the year with a decline in client hours when compared to the previous year. This was, as explained above, due to changes in our funder’s assessment policies whereby only whānau with the greatest of healthcare needs could be assessed for funding.
By halfway through the year, however, we were back to where we started and finished the year with an increase in client hours. Much of this increase has been due to an increase in the complexity of need presenting in our current case loads.
Individualised Funding – a Rewarding Outcome
One of the most rewarding outcomes of the year has been the significant development of our Individualised Funding host service practices and as a result the large number of compliments we are receiving about how we support Individualised Funding users and their whānau. We have managed to hold people well despite the changes to the IF guidelines .
Individualised Funding (IF) enables a person with a disability (and their whānau) to decide how they are supported, what support they access, who provides their support and when it happens. This can involve the person purchasing disability supports or employing their own Support Workers. People using IF have a personalised budget for disability supports and are supported by an IF host provider in how they use their funding.
It has been a challenging year for the disabled community using Individualised Funding because the rules governing what people could use their funding on were made more restrictive by disability support services. This has led to significant disappointment amongst the disabled community and made our work to hold our disabled clients more important, continuing our work to persuade funders and stakeholders to meet their needs more fully, especially for those with increasing complexities.
Our skilled IF Team have provided significant support this year to assist people to use their personalised budgets and to support them to overcome any barriers they face in living in the community. This has included assisting people with specialised information, linking them to other social and navigational support in the health, disability and social support systems.
In many cases the support that we are providing through our IF Host Services is greater than what we are contracted to deliver, however the care we provide is aligned to our values and shows our deep commitment to providing an integrated approach that works for all.
Amelia’s Story
Life as the parent of a child with complex specialised needs can be overwhelming, especially when you don’t know what support is available. “I didn’t know anything about Individualised Funding or the help that was out there for me and Peter,” she explains. “Life was hard because I thought I had to do it all myself.”
Complexity and Demographics
Across all our services, we are seeing greater complexity of need.
Due to people living in their own home longer, the needs of the clients we support has increased.
Alongside the increase in the acuity of need, is an increase in the presentation of a range of other complexities.
Mental health challenges and vulnerable social situations are common across the whānau we support. Many of these needs are either unfunded or not being accessed through existing systems, leaving individuals and families to fall through the cracks in our health and social services.
To ensure our support workers can provide safe, effective, and goal-oriented care, our teams are regularly connecting whānau with a wide range of external services. These include food support, housing, relationship counselling, and mental health services—often in complex combinations.
This growing complexity means our support workers and clinical teams are spending significantly more time with each client. The average hours per client have steadily risen, and this upward trend is being tracked year-on-year. As the needs of our home healthcare clients continue to deepen, we expect this trajectory to persist.

The age demographics of our clients are also interesting. The average age of our clients, excluding Individualised Funding is 80 years old. The average age of those in our Individualised Funding service is 30 years old.
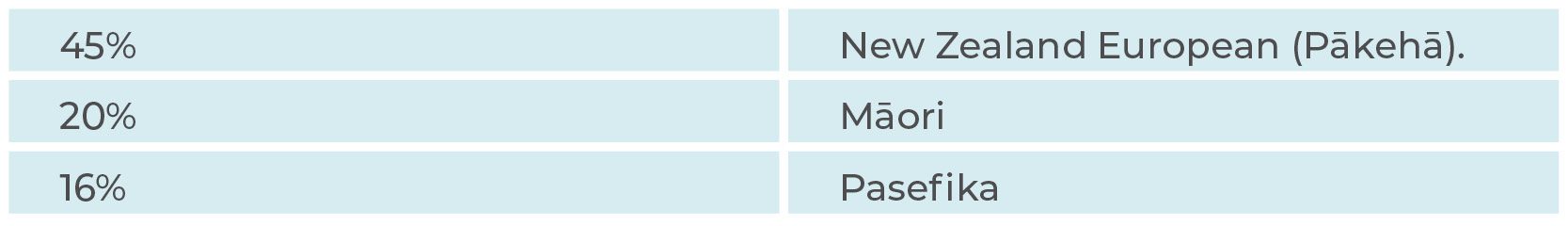
Ethnically, the general Home Healthcare clients are:
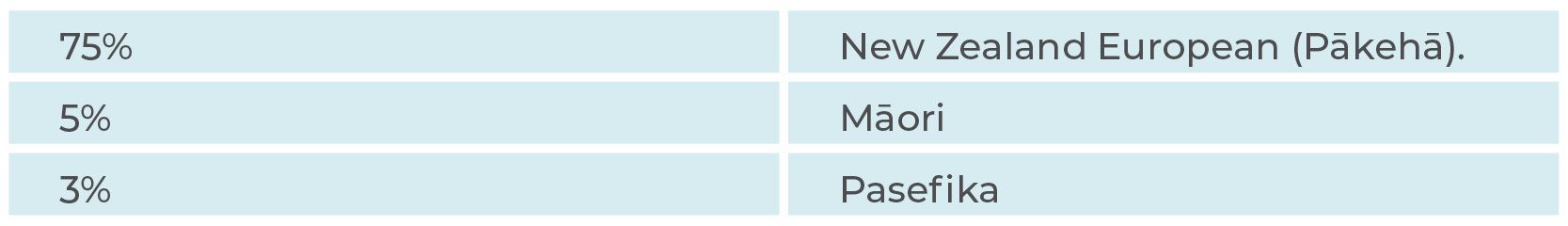
Amongst our IF clients the ethnic breakdown is:
Support Worker Marketing Campaign photo shoot.
Certification Audit – Completed
Every 18-months, home healthcare providers undergo a ‘Surveillance Audit.’ Then, every three years, they must undergo a full ‘Certification Audit’. This past year, Visionwest Home Healthcare completed our first full Certification Audit under the new standard – Ngā Paerewa. It was encouraging to staff that the Audit was passed with no areas of concerns or recommendations for change.
Conclusion
In the midst of a year with some very real challenges, Visionwest Home Healthcare has again excelled in providing in-home support to a growing number of clients. The ACC Maximise Independence contract and the development in Individualised Funding, while adding to the complexity of client need, means our client numbers and client hours should both continue to increase in the coming year.
The important thing for the Home Healthcare team is that we are well positioned to continue to deliver quality home healthcare to those who so greatly need it.
People supported
Hours of support delivered
While total Support Worker numbers are relatively static (1,278 to 1,297), the team in Rotorua has grown by 24.3% (70 to 87 Support Workers) in one year. This supports the 30% growth in hours that we are delivering in this region.
Alexander’s Story
At 61, Alexander felt a sudden, alarming pain in his chest. He was rushed to Waikato Hospital for emergency surgery. After surgery Alexander faced uncertainty about managing recovery alone, At this critical moment, he turned to Visionwest.